John didn’t start his career mad.
He trained as an emergency medicine doctor in a tidily run Midwestern emergency room about a decade ago. He loved the place, especially the way its management was so responsive to the doctors’ needs, offering extra staffing when things got busy and paid administrative time for teaching other trainees. Doctors provided most of the care, occasionally overseeing the work of nurse practitioners and physician associates. He signed on to start there full-time shortly after finishing his residency.
A month before his start date, a private equity firm bought the practice. “I can’t even tell you how quickly it changed,” John says. The ratio of doctors to other clinicians flipped, shrinking doctor hours to a minimum as the firm moved to save on salaries.
John — who is being referred to by a pseudonym due to concerns over professional repercussions — quit and found a job at another emergency room in a different state. It too soon sold out to the same private equity firm. Then it happened again, and then again. Small emergency rooms “kept getting gobbled up by these gigantic corporations so fast,” he said. By the time doctors tried to jump ship to another ER, “they were already sold out.”
At all of the private equity-acquired ERs where John worked, things changed almost overnight: In addition to having their hours cut, doctors were docked pay if they didn’t evaluate new arrivals within 25 minutes of them walking through the door, leading to hasty orders for “kitchen sink” workups geared mostly toward productivity — not toward real cost-effectiveness or diagnostic precision. Amid all of this, cuts to their hours when ER volumes were low meant John and his colleagues’ pay was all over the place.
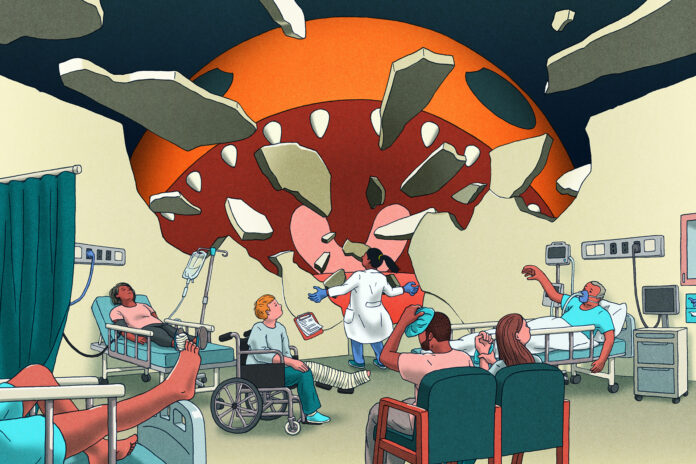
Patient care was suffering “from the toe sprains all the way up to the gunshot wounds and heart attacks,” says John. His experience wasn’t an anomaly — it was happening in emergency rooms across the country. “All of my colleagues were experiencing the same thing.”
“Were they going to die anyway? Maybe. But that’s not how I sleep at night. That was four years ago. I think about that guy every day.”
At times, the short staffing combined with the pressure to churn patients led to deadly shortcuts. John remembers rushing to evaluate one patient and missing his extensive history of alcohol abuse. The patient spent hours getting tests directed at the wrong diagnosis.
John could have put together a more appropriate plan if he’d had a few more minutes to sit down and get a better history, but by the time he realized what was going on, the patient was too severely ill. He died in the intensive care unit two days later.
“Is that 100 percent because of that staffing? Probably not,” says John. “But if I wasn’t so stressed about jumping into that patient room, making sure my door-to-provider time was less than 25 minutes …” The hypothetical hangs in the air.
“Were they going to die anyway? Maybe. But that’s not how I sleep at night. That was four years ago. I think about that guy every day.”

The story of how private equity has been able to so thoroughly debilitate emergency care is one of the more dramatic examples of how corporate interests are corrosive to America’s health care system — and how powerless they leave individual consumers. Today, private equity continues to operate a shocking quarter of ERs nationwide, as of March 2024.
Still, there’s some hope: Academics, patient advocates, and doctors say you can make defensive moves to protect your finances and care before, during, and after you or a loved one visits an ER.
Understanding private equity’s transformation of America’s emergency rooms is the first step.
How private equity sunk its claws into emergency care
Modern private equity got its start in the early 1980s, when a free-market acolyte — and former member of the Nixon administration — completed the first major “leveraged buyout.” Using mostly borrowed money, William Simon and his partner bought a greeting card company, extracted huge fees, and then sold it for a massive profit less than two years later.
Over the next few decades, what was then called the leveraged buyout industry moved into other sectors. Firms flipped businesses to yield spectacular profits, often cutting corners on the products and services they offered, eliminating jobs, and reducing employee benefits.
It was only a matter of time until the industry, now rebranded as private equity, turned its gaze on the US’s $4 trillion health care sector, which was already becoming increasingly commercialized as nonprofit health systems consolidated, paid their executives ever more extravagant salaries, and otherwise played business hardball. Private equity takeovers in health care started around 2000 and have steadily increased since; when several big banks crumbled in the wake of the 2008 financial crisis, private equity’s growth only accelerated.
Emergency medicine wasn’t always an appealing target for private equity. Physician staffing in many emergency rooms around the country was traditionally handled by co-op-like groups, run by working doctors, that contracted with hospitals. In the 1990s, ex-physicians and businesspeople began taking ownership of these so-called contract management groups (CMGs). As they did, they started acting more like for-profit businesses, centralizing decision-making and earnings.
The easier it was to make decisions that prioritized profits, the more money CMGs made — and the more attractive they became to private equity.
Through the mid- to late-2010s, private equity firms swallowed up a shocking number of American emergency rooms, leaving in their wake a generationally hollowed-out system for providing emergency care to people across the country. Private equity firms and other corporate interests owned nearly 9 percent of ER doctor groups in 2009; by 2019, they owned 22 percent. The wave of takeovers and consolidations peaked in 2021 but carries on all over the US, especially in Florida, Texas, and other parts of the South and West where the firms have been most aggressive.
Doctors trying to practice medicine the way they’d been trained to — with a priority on patient care, not profits — found they couldn’t outrun the monster. Private equity’s dominance persisted even after the federal No Surprises Act, enacted in 2022, made many of their most profitable practices illegal.
Lots of for-profit models are a bad fit for health care, but of all of them, private equity is perhaps the worst, says Eileen O’Grady, director of programs at the Private Equity Stakeholder Project, a nonprofit watchdog group: “It basically takes the for-profit model and makes it so much more extractive and so much more harmful and risky.”
Private equity puts profit above all else
To understand what makes private equity such a malignant force in health care, you have to understand its uniquely craven and purposefully opaque corporate structure.
Imagine you own a lemonade stand, and you want it to make more money. You have a few options: You can plow all your profits back into the business until it grows — what business school types call organic growth. Alternatively, you can get a bank loan. If you’re really ambitious, you can sell shares of your lemonade stand to the general public by promising them a good return on their investment.
There’s another option here, one that will make you richer quicker: You can sell all or most of the stand to the rich kid at the end of the street. He’s offering you a lot of money for it — more than you’d get over the short term from the other options. That’s because he’s taken out a huge loan to pay for the deal.
But there are a couple of catches: First, if he runs into financial trouble (which he very well might, since he’s been buying up lemonade stands all over town), he’ll sell it off for parts, leaving the neighborhood lemonade-less. This will cost him nothing personally because he used the lemonade stand as collateral for that big loan.
The second and perhaps more important catch is that this kid is buying your lemonade stand in order to sell it. He doesn’t care about lemonade or the people who like it. His strategy is to make the stand’s balance sheet look so attractive that a few years later, another investor will buy it at a premium — or if that fails, then yes, to sell it off for parts. A year down the road, odds are high your precious lemonade stand will be a sad shadow of what it once was, or it might not exist at all.
That kid is private equity.

When private equity comes for a lemonade stand (or for Toys “R” Us, Samsonite, Mitchell Gold + Bob Williams, or for any of the thousands of businesses these firms have taken over since they rose to prominence in the late 1980s), the result is often a sad story about the decline of a legacy brand — shoddy products and lost jobs. Depressing, but not a life-and-death issue. When private equity comes for health care, though, the result is human suffering: Elderly and intellectually disabled people sitting in puddles of their own waste, sick patients not getting the care they need, worse outcomes for patients. It’s not just lemonade. People’s lives are at stake.
The way private equity gets into emergency care is by buying out the CMGs that manage physician staffing — that is to say, the firms only buy the clinicians themselves.
It’s a different model than when private equity invests in other areas of health care. When firms buy hospitals, nursing homes, medical practices, rehabilitation facilities, and group homes, they acquire not only staff, but also buildings, land, and medical equipment.
In the case of emergency care, “private equity doesn’t pay the hospital rent, they don’t hire the nurses, they don’t pay the electric bills, they don’t provide any of the equipment,” says Robert McNamara, chair of the emergency medicine department at Temple University in Philadelphia. The hospital still handles those finances. “They’re just working the labor force. … The highest-cost thing on their expense side is the board-certified emergency physician.”
When emergency rooms first caught the eye of private equity firms, the prospective investors offered the physician owners of CMGs huge payouts.
Leon Adelman, an emergency medicine doctor who leads the staffing firm Ivy Clinicians and writes a workforce-focused newsletter, says the owners faced a tough choice: “‘Do I do what is ethical and feels right … and I get a nice going-away party and maybe a watch or something — or do I get $10 million?’”
“What they were buying was the ability to charge patients who were consuming a non-shoppable service,” Adelman says — one for which patients are unable to compare prices. If you’re having a heart attack, you’re not going to call around to hospitals to find out who is going to give you the best deal.
Hospitals that increasingly have profit on the brain often found private equity a more attractive partner than doctor-owned CMGs. The firms are flush with cash, which means they don’t look to the hospitals to shore up their finances. “They won’t ask you for a penny,” Adelman explains. “They’re making plenty of money.”
Once a private equity firm bought an emergency room, there were two levers it could pull to make a profit: It could maximize what it reaped from patients who’d received services, and it could cut what it spent paying the clinicians who provided those services.
Doing both at the same time has made emergency medicine practically unrecognizable.
Burned-out doctors, screwed-over patients
Under new private equity ownership, ERs adopted an assortment of unsavory practices. Firms not only pressured clinicians to see patients faster, as illustrated by John’s experience, but to recommend hospital admission for more patients. They also dramatically raised the price tags for a range of emergency services, resulting in back-breakingly large bills for patients nationwide, like ones charging thousands of dollars for glue applied to a half-inch wound.
To avoid having to negotiate those astronomical bills with the expert hagglers at insurance companies, firms kept their ERs from participating in many insurance networks. It was easier to collect on a so-called balance bill — the portion of a medical bill not paid for by a patient’s insurer — if the care a patient had received wasn’t covered by their insurance at all.
In a study of two of the largest emergency medicine staffing firms in the US, health economist Zack Cooper found costs to patients went up more than 80 percent after a corporate interest took ownership.

Meanwhile, to minimize costs, private equity-owned staffing firms often replaced more expensive physicians with nurse practitioners and physician associates. It was a move likely to worsen patient care: While these professionals do highly skilled work in a variety of clinical settings, the emergency department is one place where care outcomes are more likely to suffer if a doctor isn’t involved.
In a demonstration of how deeply invested private equity was in emergency care, these firms set in motion a system to generate cheap labor, trained to private equity’s productivity maximizing specifications. For-profit health care companies, including private equity-invested ones, founded a glut of residency training programs in the late 2010s. A 2021 study projected the move would lead to an oversupply of more than 7,800 emergency medicine doctors by 2030. According to reporting by Lever, the private equity-funded staffing firm American Physician Partners told investors they expected the surplus to eventually save them an expected $20 million in annual payroll costs.
There are good reasons to believe that private equity’s soup-to-nuts transformation of emergency care has had a devastating effect on physician morale and patient care — and many emergency doctors say both are true. In lemonade-stand terms, private equity is “diluting the lemonade, but charging six times as much,” Adelman says, and their customers are “dying of thirst.”
Emergency medicine has long been among the most stressful physician specialties. However, in recent years, the burnout rate has climbed to 63 percent, according to a 2024 Medscape survey, and the specialty is losing popularity among medical students. Doctors’ decision-making authority is their currency; “To have that taken away because of leadership and ownership models that negate that authority is really disheartening, and leads to burnout and, really, moral injury,” says Aisha Terry, a Washington, DC, emergency room doctor and president of the American College of Emergency Physicians, an advocacy and education nonprofit.
In lemonade-stand terms, private equity is “diluting the lemonade, but charging six times as much,” Adelman says, and their customers are “dying of thirst”
Meanwhile, finding concrete data proving patient harms is difficult. Yashaswini Singh, a health care economist who studies changes in physician practices acquired by private equity funds, says linking patient outcomes with private equity involvement is “a Herculean task.” Still, researchers are on the case, and so are legislators — earlier this year, Sen. Gary Peters (D-MI) initiated an investigation into private equity’s effects on the quality of emergency care.
Private equity can only do what it does because so many other parts of American health care are so dysfunctional. “Just to be really clear, private equity is not the main harm of health care in the US,” says O’Grady. “I think it’s a symptom of a much bigger problem.”
In the US health care ecosystem, private equity is a bottom-feeder, an entity that can only exist because of the bad behavior and misaligned incentives of the bigger players in the marketplace. Private equity’s deep pockets, its willingness to extort patients, its heavy-handedness with telling doctors how to practice wouldn’t be possible — much less an advantage — in the absence of these larger upstream problems.
Maybe there wouldn’t be as many opportunities for private equity to make money in health care if hospital budgets were stable; if insurance companies didn’t play hardball with both providers and patients; if pharmaceutical industry players didn’t artificially and unevenly inflate drug prices; if elected officials weren’t so susceptible to powerful lobbies that block comprehensive, loophole-closing health care reform.
That’s not the world we live in, however; and because the American health care system is broken in these and so many other ways, private equity thrives within it, often invisibly.
Congress tried to fix the problem — but fell short
In 2020, Congress threw a huge wrench in the private equity game plan when it passed the No Surprises Act, aimed at saving patients from receiving shocking bills after getting emergency care.
When the law took effect in January 2022, it meant that patients who receive emergency care can’t get billed for out-of-network care, even if the care is from an out-of-network facility or doctor. (They do still have to pay whatever deductibles, copays, or coinsurance their insurance plan would require related to an in-network visit.) It also protects people from higher bills if they get routine, non-emergency care at an in-network facility from an out-of-network doctor without their knowledge or consent.
Billers — including private equity owners of emergency medicine practices — now have to ask insurance companies to pay the balance of their out-of-network bills. It turns out it’s a lot harder to extract unreasonable fees from insurance companies than from individuals.
The act served as the death (or near–death) blow for several emergency medicine groups backed by private equity, which at their peak staffed nearly one-fifth of American emergency departments. That really only means some of these firms are now being run with oversight from courts and creditors, not that all of them are out of business: They’re largely still standing, and many have since only expanded their footprint in emergency care.

The No Surprises Act did some good for people, but it’s far from perfect. Many people simply are unaware when they’ve been incorrectly billed. Clinicians and the facilities they work for occasionally don’t follow the legislation’s rules, or inappropriately ask patients to waive their protections. Insurance companies don’t automatically absolve patients of responsibility for a surprise out-of-network bill, and the appeals process is complicated and time-consuming. And there are loopholes: Out-of-network ambulances and urgent care facilities aren’t covered, and neither is the follow-up care people get after an emergency room visit.
The emergency medicine profession, meanwhile, will take a while to recover from private equity’s onslaught. John’s colleagues are the kinds of doctors who will drive a patient home if they don’t have a ride, he says. Many of the people who seek care in American emergency rooms live on the poorest and most marginalized fringes of society; emergency medicine doctors know this, and for some of them, it’s an important reason they chose the work.
“This is not about pay for us,” he says. “This is just about being fair and letting us practice how we want to practice. And that’s gone.”
What to do when you need emergency care
It has to be said: Patients shouldn’t have to be shrewd when navigating a system that’s supposed to care for them at their most vulnerable, or risk both their life and their finances. And yet, that’s the health care system the US has.
It’s hard for people to tell when a private equity firm has taken over a local emergency room. It’s not like the firm slaps its logo on the side of the building. Patients usually don’t even know until they get a bill that an investment company had a hand in determining who saw them in the emergency room and what kind of workup they ordered, says McNamara.
Given that reality, anyone who may one day visit an emergency room in the middle of a crisis — that is to say, nearly everyone — should know how to protect themselves, says Patricia Kelmar, who directs health care campaigns for the Public Interest Research Group (PIRG). There are things you can do to ensure you don’t end up with an astronomical bill.
Know where to go and who is treating you
Some situations don’t permit much decision-making about which emergency room you’ll go to or how you’ll get there. Still, it’s worth making an advance plan for where you’ll go if you have the option.
Cooper, the health economist, says an emergency room’s ownership isn’t the only thing that matters in deciding whether to go there in an emergency. If a private equity-owned ER sees a higher patient volume than others and is affiliated with an academic institution, it may still be the best option.
Even with the No Surprises Act in place, care from in-network doctors at in-network hospitals is far less likely to result in unpleasant bills. So before you need an emergency room, check with your insurance company to see which ones are in network and nearest to you. Once you’re at an emergency room, Cooper suggests asking to see an in-network physician.
Make a plan for how to get there
Ambulance transport is unlikely to be cost-free for most Americans, so if you need to get to an emergency room and you’re in stable condition, it’s worth trying to get there in other ways.
Air ambulances are covered by the No Surprises Act, but ground ambulances are not, and are unfortunately often out-of-network for many people. The ones owned by private equity are especially likely to be wildly expensive. Nevertheless, many states have laws to protect consumers from outrageous ambulance bills — but only if their plan is state-regulated, which means about 60 percent of insured people are still unprotected. You can figure out if yours is one of them by contacting your state’s insurance department.
You can also work with your insurance company and the ambulance company to negotiate big bills; legal aid organizations can also provide assistance.
Understand what you’re signing
Non-emergency hospital departments (for example, the ones that would take care of you if you had to stay in the hospital for more care after an ER visit) are allowed to ask you to sign away your No Surprises Act protections. The form they use to do this is, totally unironically, called a Surprise Billing Protection Form.
Emergency rooms, however, aren’t allowed to ask you to sign this waiver. If they do, say no and report the violation to the No Surprises Help Desk by calling 1-800-985-3059. Almost every US hospital still has to provide care for you under US law.
If you get a wonky bill, file a complaint
If you do still end up with a nonsensically large bill, you can push back and appeal decisions — again, by reaching out to the No Surprises Help Desk.
Additional guidance on your medical billing rights is available on the PIRG website, and legal and other help may be available from organizations like Dollar For and local legal aid groups.
Demand better from community leaders and elected officials
There are better approaches to solving emergency medicine’s problems than by doing hand-to-hand combat with private equity’s worst practices. Reducing the overall harm requires change on a systemic level.
Zirui Song, a Harvard health economist and internist who studies private equity in health care, says those changes include better enforcement of the laws we have aimed at preventing consolidation, fraud, and abuse; closing tax loopholes and other laws that allow private equity firms to conduct business while taking on minimal financial risk; and requiring transparency around private equity health care acquisitions and health care prices. These are all subjects you can contact your elected officials about.
You can also ask to join the board of your local hospital, says McNamara. At nonprofit health systems in particular, these groups are required to include people from the community. As a member, you could learn more about how private equity works and say, “We don’t want private equity in our community.”
This story is supported by a grant from the National Institute for Health Care Management. Vox Media had full discretion over the content of this reporting.